Not So Common Immune Deficiencies
Allergies and asthma affect millions of people worldwide. While most cases are due to environmental factors, some people may have underlying immune deficiencies that contribute to their symptoms.
Common immunodeficiencies such as allergies and asthma can be treated with lifestyle changes and medications, but rare immunodeficiencies require careful monitoring and treatment to ensure long-term health and well-being.
Multidisciplinary Snot Force Alliance Webcast with Allergist Dr. Lee S. Clore
In May 2023, the Snot Force Assemble! CME webcast delved into the topic of Not So Common Immune Deficiencies, led by Dr. Lee S. Clore, esteemed owner of Allergy and Asthma Specialists, PSC. This case-based event brought together a diverse range of specialists, including otolaryngologists and allergists, to collectively explore the intricacies of managing these unique conditions. Attendees had the opportunity to share and exchange insights on the management and treatment strategies for challenging cases, enhancing their knowledge and expertise in this field.
Keep reading to take a look at some of the rare immunodeficiencies that may be related to allergies and asthma and discuss how they can be managed.
Common Variable Immunodeficiency
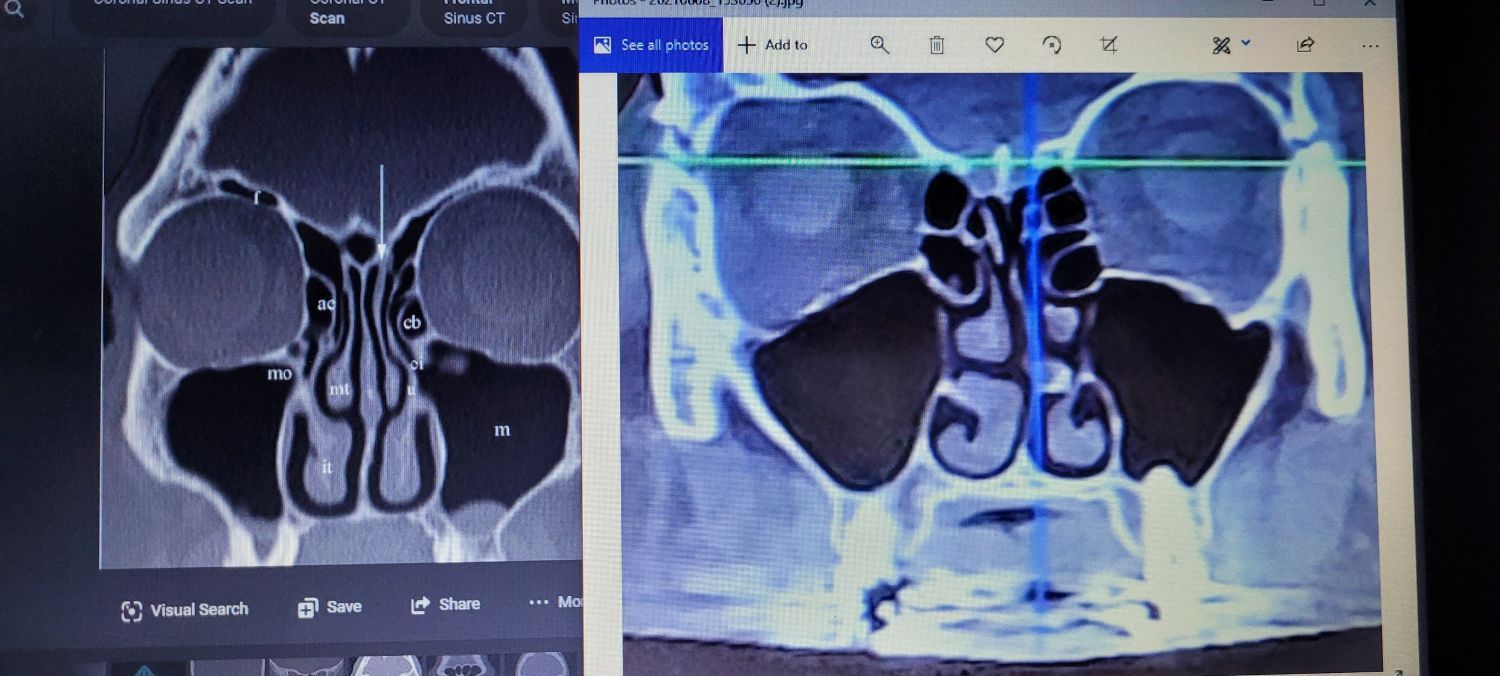
Common Variable Immunodeficiency (CVID) is a primary disorder characterized by low levels of immunoglobulins in the blood. This condition affects both males and females equally and is typically diagnosed in adulthood. Patients with CVID may experience sinusitis, ear infections, gastrointestinal infections, recurrent infections, autoimmune disorders, allergies, and asthma.
The diagnosis and management of CVID require specialized testing and treatment by an experienced immunologist.
Primary Immunodeficiency
Your body's immune system aids in combating infections. Individuals with primary immunodeficiency (PI) have a malfunctioning immune system, which makes them more susceptible to contracting infections and experiencing severe illness as a result.
There are over 400 types of PI, which vary in severity. Some individuals may not discover their mild form of PI until adulthood, while others may experience complications from birth or infancy. There is also a more unusual type of PI known as Activated PI3 kinase delta syndrome (APDS).
Activated PI3 Kinase Delta Syndrome (APDS)
This is an uncommon genetic disorder that was recognized as a primary immunodeficiency disease not so long ago. There are two forms of APDS: APDS1 and APDS2, which are both hereditary.
The disease disrupts the functioning of the immune system. The primary indications of APDS include recurrent infections in the upper respiratory tract, sinuses, ears, bronchitis, and pneumonia (a lung infection). While most individuals with APDS encounter their initial infection during early childhood, symptoms can appear at any age.
Additional symptoms include irritation in the gastrointestinal tract, swelling of lymph nodes, enlargement of the liver and spleen, and an elevated risk of developing lymphoma. Prolonged ear and respiratory tract infections can eventually result in permanent hearing loss and the formation of scar tissue in the lungs, known as bronchiectasis.
Treatment for APDS revolves around symptom management, infection prevention, and inflammation reduction.
Treatments
Scientists are making brilliant advancements in developing new treatments for immune deficiencies. Recently, JOENJA® (leniolisib) has been approved by the FDA to treat activated phosphoinositide 3-kinase delta (PI3Kδ) syndrome (APDS) in adults and children 12 years of age and older.
Other treatments for immune deficiencies include immunoglobulin replacement therapy, bronchodilators, immunomodulatory drugs, and anti-IgE therapy.
In this article, we have only touched the surface of the immunodeficiencies related to allergies and asthma. Learn more about immunodeficiencies and other conditions related to the airways from the Snot Force Alliance.
Our webcast series on “Not So Common Immune Deficiency” brought together experts in the field to discuss the latest research and advancements in diagnosing and treating immunodeficiencies. Join the force today to participate in our next meeting and get more insights about such complex disorders. Contact us for more details.