From Heartburn to Hoarseness: Distinguishing Between GERD and LPR in Clinical Practice
Gastroesophageal reflux disease (GERD) and laryngopharyngeal reflux (LPR) are two conditions that healthcare professionals frequently encounter in clinical practice. While both are characterized by the backflow of stomach contents into the esophagus, distinguishing between GERD and LPR is important for accurate diagnosis and effective management strategies.
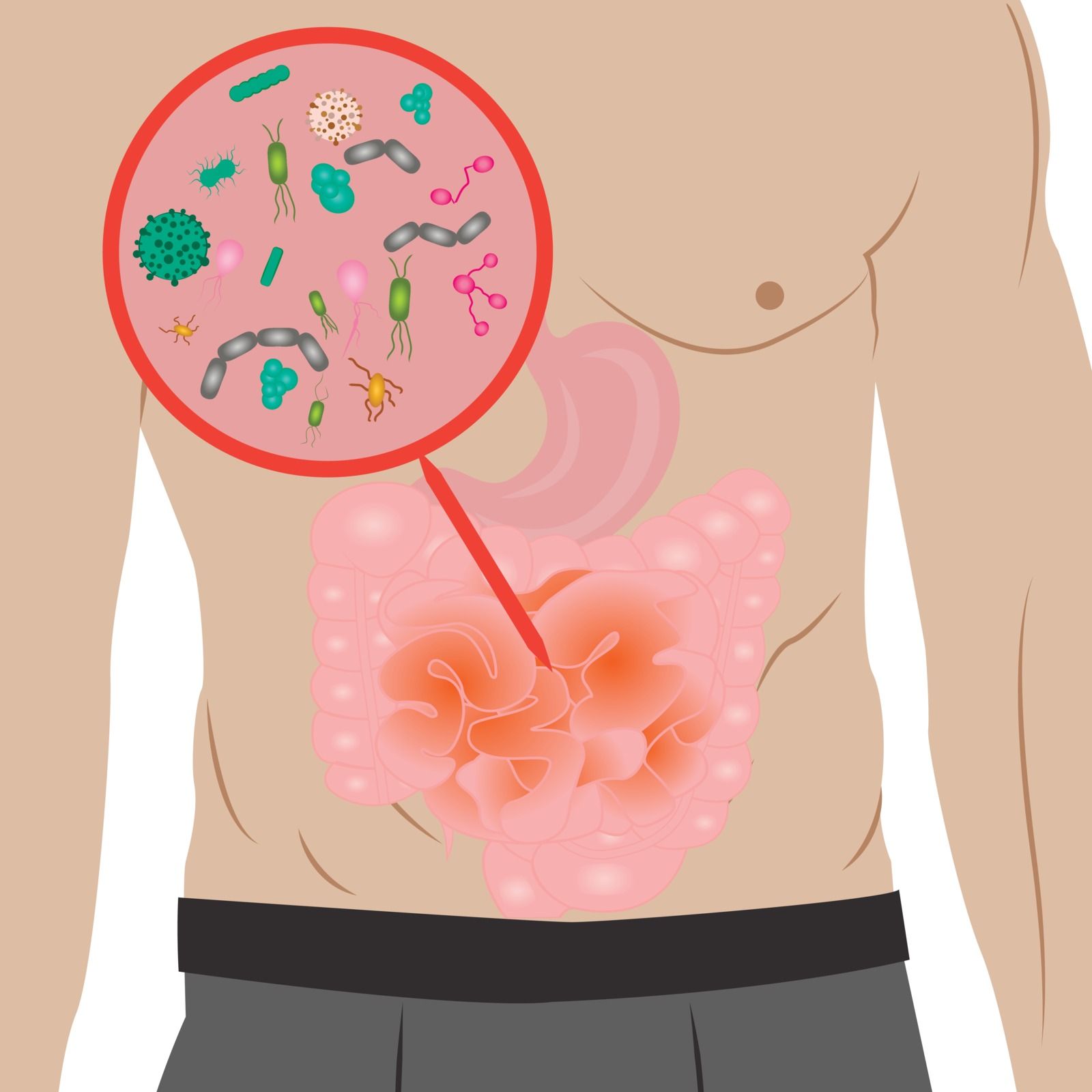
GERD Pathophysiology
GERD is primarily caused by lower esophageal sphincter dysfunction, allowing stomach acid to reflux into the esophagus, leading to mucosal injury and inflammation. Factors such as obesity, hiatal hernia, and dietary habits contribute to GERD.
LPR Pathophysiology
LPR involves reflux beyond the upper esophageal sphincter into the larynx and pharynx, irritating the mucosa and causing symptoms like hoarseness, the feeling of something stuck in the throat, and chronic cough. Impaired upper esophageal sphincter function and anatomical factors play a role in LPR development.
Differentiating Mechanisms
While both conditions share reflux as a common mechanism, their clinical presentations differ due to the localization of refluxate exposure. GERD affects the lower esophagus, while LPR targets the upper aerodigestive tract.
Impact on Tissue Integrity
GERD can lead to erosions, ulcers, and Barrett's esophagus, while LPR may cause hoarseness, chronic cough, globus (the feeling of something stuck in the throat), postnasal drip, vocal cord edema, and laryngeal complications. The anatomical locations of reflux injury influence clinical profiles and complications.
Clinical Implications
Differentiating between GERD and LPR can be challenging due to overlapping symptoms. While heartburn is a hallmark feature of GERD, it is less common in LPR. Healthcare professionals must consider atypical symptoms like hoarseness and chronic cough in diagnosing LPR, as these may not be as readily apparent as typical GERD symptoms.
Diagnostic Approaches
Accurate diagnosis of GERD and LPR requires a comprehensive evaluation. Endoscopy can visualize esophageal mucosal changes indicative of GERD, while laryngeal examination, pH monitoring, and laryngoscopy are essential for diagnosing LPR. Thorough assessment and a high index of suspicion are vital in distinguishing between these conditions.
Collaborative Care Approach
Effective management of GERD and LPR necessitates collaboration among healthcare professionals from various specialties. Otolaryngologists, gastroenterologists, speech therapists, and dietitians all play critical roles in comprehensive patient care. Regular follow-up assessments and patient education are integral for optimizing treatment outcomes.
Recognizing the distinctions between GERD and LPR is essential for healthcare professionals to effectively diagnose and manage these reflux-related conditions. Discussion and collaboration with others in similar fields can give practical and insightful information, and
Snot Force Alliance
is just the right place. Snot Force brings multidisciplinary specialists together to inspire innovation to manage the inflammatory disease of the airway medically.
Join the team today!